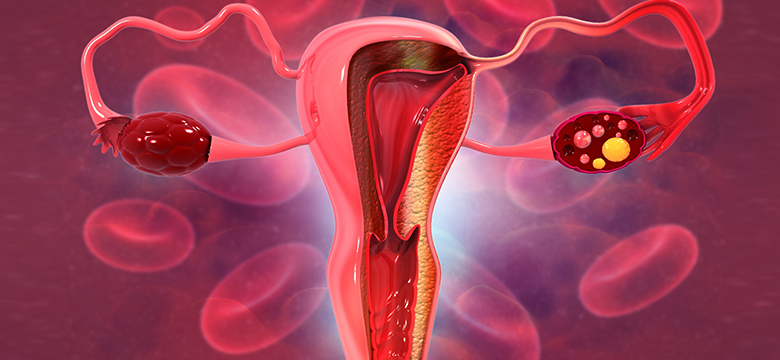
Egg freezing, also known as oocyte cryopreservation, is a revolutionary procedure that allows women to preserve their fertility for future family planning. Whether focused on your career, pursuing higher education, or not ready for parenthood, egg freezing allows you to choose when to start your family.
Egg freezing involves collecting a woman’s eggs, freezing them and then thawing them later for fertility treatment.
Who Can Benefit from Egg Freezing?
Egg freezing is an excellent option to preserve a woman’s fertility for various scenarios, including;
- Undergoing medical treatments that may affect fertility.
- The presence of a disease that requires removal of the ovaries
- A family history of early menopause.
- For women prioritising their career or education and thus seeking to delay parenthood.
Understanding the Egg Freezing Process
Egg freezing involves extracting and freezing a woman’s eggs to preserve their quality and viability for future use. Here’s an overview of the process:
1 – Consultation
Your journey begins with a consultation with one of our fertility experts, where we’ll discuss your goals, assess your fertility status, and create a customised plan.
2 – Ovarian stimulation phase
- Once we pass this stage and have a clear profile of your status and medical history, our fertility specialist will prepare your medication protocol.
- You’ll start your ovarian stimulation phase from the 2nd day of your menstrual cycle and continue for approximately 10-14 days. During this phase, you’ll take stimulation medicines and injections from our medical team with multiple ultrasound checkups to monitor your ovaries’ progress.
- Once our doctor confirms the follicles have reached the targeted size, the stimulation phase ends, and you are prepared for the IUI procedure. We will inform you about the exact timing of the trigger injection to help release the eggs.
3 – Egg Retrieval
- When the eggs are mature, the stimulation phase ends, and you undergo the egg retrieval procedure.
- The egg retrieval (OPU) procedure is performed using sedation (anaesthesia) at our hospital, which takes approximately 15-20 mins.
- After the egg retrieval procedure, you will be informed about the number and quality of eggs collected.
4 – Egg Freezing
The harvested eggs are carefully frozen and stored in our secure facility. The vitrification method is used at our hospital to freeze the eggs.
5 – Future Use
You can decide when and how to use your frozen eggs for assisted reproduction, in vitro fertilisation (IVF), or other fertility treatments.
Take Control of Your Fertility
At Cyprus IVF Hospital, we’re here to support you every step of the way on your fertility journey. Egg freezing is not just about preserving eggs; it’s about preserving your choices and giving you the flexibility to start a family when the time is right.
Contact us today to schedule a consultation and learn how egg freezing can be a game-changer in your family planning journey.
Frequently Asked Questions About Egg Freezing
If I freeze my eggs, will my future baby be normal?
Many healthy live births have occurred since the first in vitro fertilisation trial with frozen oocytes in 1986.
Research on the health of children born through in vitro fertilisation has shown no increase in the risk of congenital anomalies in babies born due to egg freezing.
One 2009 study that tracked 900 babies born using frozen eggs found no difference in the rate of birth abnormalities compared with the rate for babies born with fresh eggs.
(Source: Article “Over 900 oocyte cryopreservation babies born with no apparent increase in congenital anomalies” https://www.rbmojournal.com/article/S1472-6483(10)60025-9/pdf)
How is egg freezing done?
At our hospital, freezing is performed with the Vitrification method (ultra-fast freezing). With this method, ice crystals that can damage cells or tissues do not occur during freezing. Thus, after freezing, the eggs are stored in long-term storage tanks.
What is the ideal age to freeze eggs?
Women’s egg reserves and quality decrease with ageing. In addition, the risk of chromosomal anomalies in eggs increases for women over 35.
Having a good number and quality of eggs increases the chance of a healthy pregnancy and the birth of a healthy baby. For this reason, it is recommended that egg collection and freezing procedures should be completed on time and be performed until age 38.
How many eggs are collected in one attempt?
Every woman is unique. So, to answer this question more precisely, an infertility specialist will need to evaluate the woman’s hormone tests (AMH, FSH, LH, etc.) and antral follicle count.
If the woman is younger than 35, 8-12 eggs can be collected in one cycle by stimulating the ovaries. If the number of eggs collected is low, the egg collection process can be repeated several times. A higher number of eggs frozen at an early age allows more embryos to be created after fertilisation, which increases the chance of pregnancy.
How many frozen eggs remain healthy when thawed?
When frozen with the vitrification method, approximately 70-90% of the eggs stay viable when thawed in the future. The point to consider here is the quality of the eggs to be suitable for freezing.
How long can my eggs be stored for use in treatment?
Frozen eggs can be stored for many years. However, you must inform our hospital and renew your consent every year. You must give your consent on the relevant consent form. Our medical team will contact you and provide the consent forms you must complete at the appropriate time.
How much does egg freezing cost?
For detailed information about the pricing, please visit our webpage: https://cyprusivfhospital.com/pricing/